How Advanced Technologies Are Making Surgery More Precise: Robotics, Lasers, MRI, and Genetic Research
Introduction: The Era of Precision Surgery
The landscape of surgery has evolved dramatically over the past two decades. Innovative technologies such as robotic systems, lasers, advanced imaging like MRI, and genetic research have transformed how surgeons approach even the most complex procedures. Each technology contributes uniquely to making surgeries more precise, less invasive, and safer for patients. In this comprehensive guide, we’ll examine how these breakthroughs work, provide real-world examples, and offer guidance for patients and healthcare providers seeking access to these advancements.
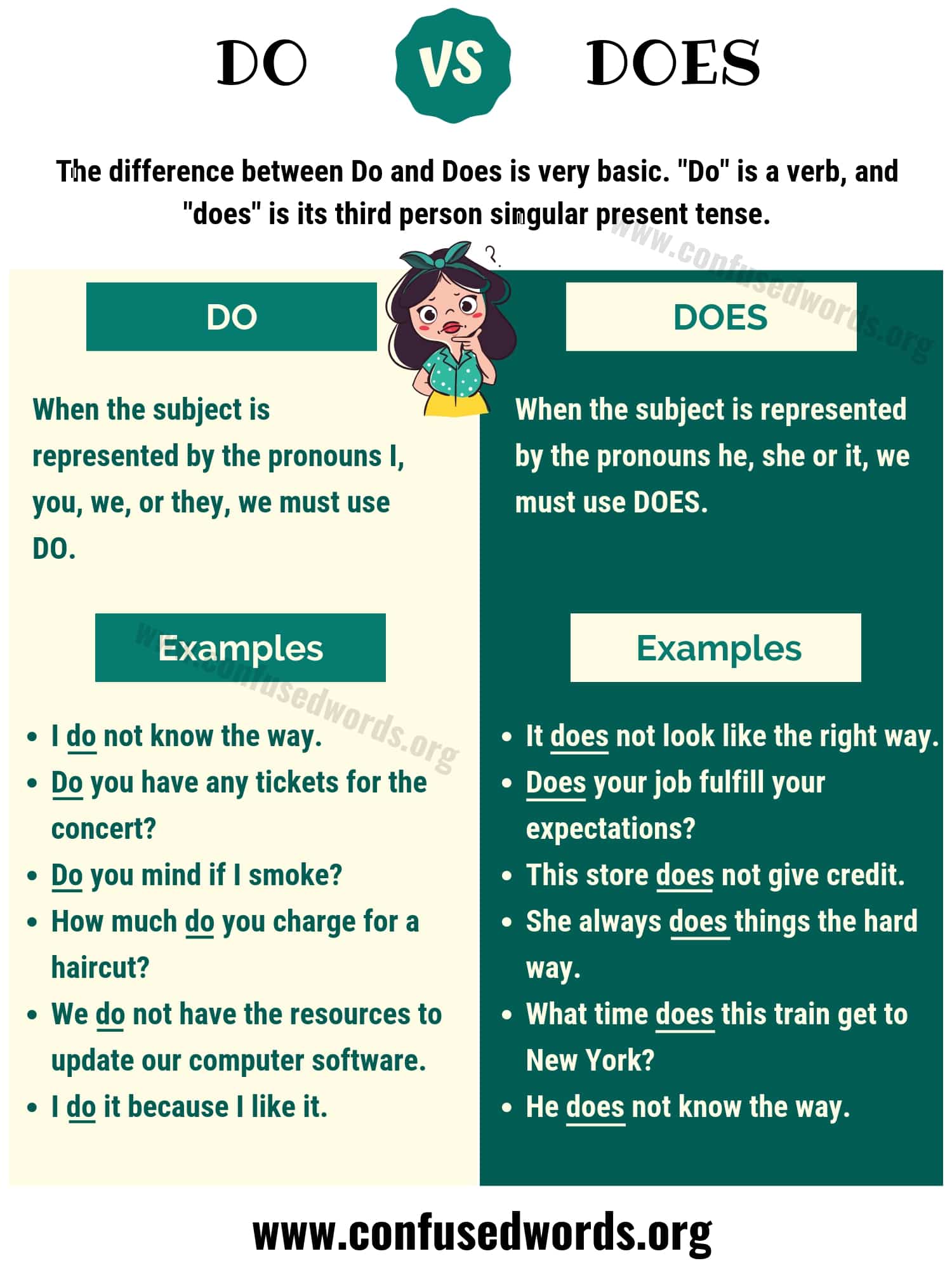
Robotic Surgery: Precision in Motion
Robotic-assisted surgery is widely recognized as a milestone in achieving unparalleled surgical precision. Systems like the Da Vinci and KangDuo robots empower surgeons to operate with enhanced accuracy and control. These robots use high-resolution 3D cameras and flexible mechanical arms that mimic a surgeon’s hand movements-often with greater range of motion and stability than human hands can achieve alone [1] , [3] .

Source: wallpaperaccess.com
For example, in procedures such as prostatectomy or radical cystectomy, robotic systems provide a magnified, 3D view of the surgical field, allowing surgeons to identify and preserve delicate nerves and tissues. The robotic arms can rotate 360 degrees, access hard-to-reach areas, and filter out hand tremors, leading to more accurate incisions and suturing [2] .
Robotic surgery typically results in:

Source: snowlenita.blogspot.com
- Smaller incisions and less tissue trauma
- Reduced blood loss and lower risk of infection
- Shorter hospital stays and faster recovery times
- Improved functional outcomes, such as urinary control or preservation of sexual function in urologic surgery
To access robotic-assisted surgical options, patients should consult with their surgical specialist and ask whether their hospital or center is equipped with these advanced systems. The American College of Surgeons and the Society of Robotic Surgery are good starting points for learning about centers offering robotic procedures. Insurance coverage may vary; patients are encouraged to contact their health provider for details on eligibility and out-of-pocket costs.
Laser Technology: Targeted Accuracy With Minimal Invasion
Lasers have long been valued for their ability to cut, coagulate, or vaporize tissue with exquisite accuracy. In surgery, this technology is used for procedures ranging from eye surgeries (like LASIK) to tumor removal and cosmetic applications. Laser beams can be finely tuned to target only the affected area, minimizing damage to surrounding tissues.
For instance, laser-assisted surgeries are standard in ophthalmology, dermatology, and oncology, where precise removal of abnormal tissue is critical. In some cases, lasers are combined with robotic systems for even greater precision. The result is reduced bleeding, lower infection risk, and faster healing for patients.
Patients interested in laser-based procedures should research accredited centers and board-certified surgeons specializing in the relevant field. The American Society for Laser Medicine and Surgery provides educational resources and directories for finding qualified practitioners.
MRI Scans: Guiding the Surgeon’s Hand
Magnetic Resonance Imaging (MRI) plays a pivotal role in preoperative planning and intraoperative navigation. High-resolution, real-time MRI imaging enables surgeons to visualize detailed anatomy, identify critical structures, and plan the most precise approach to surgery. During certain operations, intraoperative MRI allows for real-time adjustments, helping surgeons remove tumors more completely while sparing healthy tissue.
For example, in brain surgery, intraoperative MRI helps neurosurgeons achieve more complete tumor resections while minimizing neurological deficits. In prostate and liver surgeries, MRI guidance ensures the accurate localization of lesions, leading to more effective and less invasive interventions.
Access to MRI-guided procedures may depend on the facility’s resources. Patients should inquire about MRI capabilities when discussing surgical plans. To find MRI-equipped surgical centers, consult with your primary care physician or specialist, and consider seeking referrals to academic medical centers or large hospitals, which often have the latest imaging technologies.
Genetic Research: Personalizing Surgical Care
Genetic research is ushering in the age of personalized, precision medicine in surgery. By analyzing a patient’s genetic profile, healthcare teams can predict responses to anesthesia, assess risks of complications, and tailor treatments to individual needs. For certain cancers, genetic testing can determine whether a tumor is likely to respond to specific therapies or whether a minimally invasive approach is feasible.
In breast cancer surgery, for instance, genomic profiling helps surgeons decide between breast-conserving surgery and mastectomy, as well as the need for lymph node removal. In orthopedic and cardiac surgery, genetic markers can inform risk stratification and optimize perioperative care.
Access to genetic testing typically begins with a referral from your primary physician or oncologist. Tests may be covered by insurance if deemed medically necessary. The National Institutes of Health and reputable academic medical centers offer information and genetic counseling services. Patients should always seek guidance from certified genetic counselors or clinical geneticists to interpret results and inform surgical decisions.
Integrating Technologies: The Future of Precise Surgery
The convergence of robotics, lasers, advanced imaging, and genetics is rapidly reshaping surgical practice. Surgeons now have access to hybrid operating rooms where robotic systems are guided by real-time MRI or CT imaging, and procedures are tailored to each patient’s unique genetic profile. Artificial intelligence and machine learning are also emerging as tools for enhancing diagnostic accuracy and intraoperative decision-making [5] .
While adoption of these technologies varies by region and institution, their growth is accelerating. Patients should ask about available innovations during surgical consultations and request referrals to centers of excellence when appropriate. As research continues, access to these technologies is expected to expand, making precision surgery a new standard of care.
Actionable Steps for Patients and Providers
For those looking to benefit from these technological advances, consider the following steps:
- Consult with specialists who are experienced in advanced surgical technologies. Ask about their training, case volume, and outcomes with robotic, laser, or MRI-guided procedures.
- Request a second opinion if you are unsure about the best surgical approach. Multidisciplinary teams in academic medical centers often offer access to the latest innovations.
- Review your insurance coverage for advanced procedures, as policies may vary. Contact your insurer directly for details and potential pre-authorization requirements.
- Seek out reputable resources for more information. For robotic surgery, the American College of Surgeons and the Society of Robotic Surgery provide up-to-date guidance. For genetic testing, look for board-certified genetic counselors or university-affiliated centers.
- Ask about ongoing clinical trials in your area, as these may provide early access to cutting-edge surgical technologies.
Potential Challenges and Solutions
Integrating advanced technologies into surgery comes with challenges, including costs, learning curves for surgeons, and unequal access across regions. Hospitals must invest in equipment and training, and patients may face insurance hurdles or travel to specialized centers. Solutions include advocating for insurance coverage of proven technologies, participating in clinical trials, and leveraging telemedicine for second opinions and preoperative planning.
Alternatives and Additional Considerations
For patients without access to the latest technologies, minimally invasive laparoscopic surgery remains a highly effective alternative. While not as advanced as robotic systems, laparoscopic techniques still offer benefits over traditional open surgery, such as smaller incisions and faster recovery. Patients should discuss all available options with their surgical team and weigh the benefits and risks based on their specific condition and medical history.
Key Takeaways
- Robotic systems, lasers, MRI imaging, and genetic research are significantly enhancing surgical precision.
- Access to these technologies may depend on location, provider resources, and insurance coverage.
- Patients should seek care from experienced, accredited centers and consult with specialists about available options.
- As technology advances, precision surgery will become more accessible and tailored to individual patient needs.
References
- [1] Cepolina, F. (2024). Review of robotic surgery platforms and end effectors. National Institutes of Health/NLM.
- [2] Nature (2025). Short-term outcomes comparison of KangDuo 2.0 and Da Vinci surgical systems.
- [3] Reddy, K. (2023). Advancements in Robotic Surgery: A Comprehensive Review. National Institutes of Health/NLM.
- [4] NTX Surgical (2023). Robotic Surgery vs Traditional Methods: A Comprehensive Comparison.
- [5] Brookline College (2023). 8 Ways Technology is Changing the Field of Surgical Technology.
MORE FROM 9scholarships.de