Understanding and Overcoming Barriers to Effective Patient Education
Introduction
Patient education is a cornerstone of quality healthcare. It empowers individuals to make informed decisions, increases treatment adherence, and enhances overall outcomes. However, despite its importance, multiple barriers can impede effective communication and education between healthcare professionals and patients. Understanding these challenges-and knowing how to overcome them-is essential for clinicians, organizations, and patients seeking better health outcomes.
1. Time Constraints and Workload
Time constraints are a prevalent barrier in patient education. Nurses and healthcare providers often face high patient loads, administrative tasks, and shift rotations that leave limited time for thorough educational discussions. Research has shown that heavy workloads and insufficient time are major factors preventing nurses from delivering effective patient education [1] . In some studies, almost 60% of nurses reported that the time required for patient education was discouraging, especially when it was not considered in their work appraisals [3] .
Implementation guidance: To address this, healthcare institutions should consider integrating patient education into routine workflows, providing dedicated time slots for education, and recognizing educational efforts in performance evaluations. Multidisciplinary collaboration can also distribute the educational burden and ensure patients receive comprehensive support.
2. Inadequate Educational Resources and Environments
Physical and environmental barriers, such as lack of private spaces, noisy or overcrowded wards, and insufficient access to educational materials, can significantly hinder patient learning. Nurses and patients alike have cited the lack of educational resources-like pamphlets, visual aids, or quiet rooms-as a major obstacle [5] . Patients with physical disabilities, vision impairments, or mobility challenges face added difficulties in accessing educational sessions or materials [2] .
Actionable steps: Healthcare providers can improve outcomes by ensuring educational materials are available in multiple formats (large print, braille, audio, video), providing wheelchair-accessible consultation spaces, and using healthcare animations or remote consultations to reach those unable to attend in-person sessions.
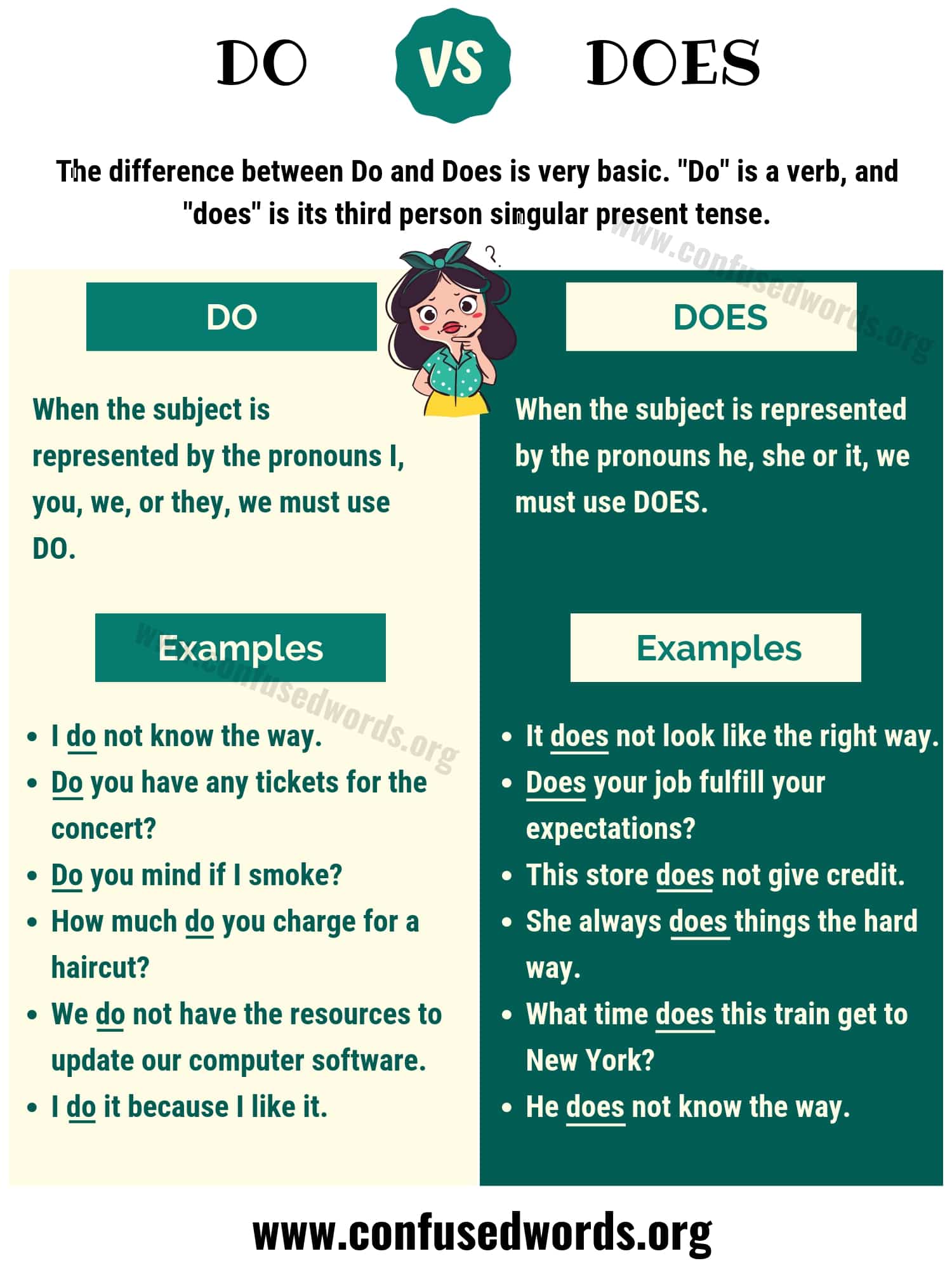
3. Health Literacy and Language Barriers
Health literacy-the ability to obtain, process, and understand basic health information-varies widely among patients. Low health literacy can result in misunderstanding of diagnoses, improper medication use, and poor health outcomes. Language differences between provider and patient are another significant barrier, especially in multicultural settings [4] . Patients who do not speak the dominant language may miss critical information or feel excluded from their care decisions.
Practical guidance: Providers can assess a patient’s health literacy using validated tools, use plain language, avoid jargon, and confirm understanding through teach-back methods. For language barriers, professional medical interpreters or multilingual educational materials should be utilized. Many hospitals now offer translated materials and interpreter services-patients can request these through their healthcare provider or patient services department.
4. Psychological and Emotional Factors
Emotional states like anxiety, fear, or lack of trust can significantly affect a patient’s ability to absorb information. Patients facing a new diagnosis, complex treatment, or hospitalization may feel overwhelmed, making it difficult to focus on educational content [2] . Trust in healthcare providers also plays a crucial role-without it, patients may not feel comfortable asking questions or expressing concerns.
Strategies for support: Building rapport, offering empathetic communication, and providing reassurance can help alleviate anxiety. Providers should encourage questions, validate feelings, and create a supportive environment to facilitate better learning. For patients with significant emotional distress, referral to counseling or mental health support services may be beneficial.

Source: venngage.com
5. Cultural and Social Differences
Cultural beliefs and social norms can influence how patients interpret health information and their willingness to engage in education. Some patients may distrust the healthcare system, prioritize traditional healing methods, or have differing attitudes toward illness and treatment [4] . These factors can impede the acceptance or understanding of medical advice.
Implementation guidance: Culturally competent care involves understanding and respecting patients’ backgrounds. Providers should ask about cultural preferences, involve family or community members when appropriate, and tailor educational content to align with cultural values. Training in cultural competence is increasingly available through hospital education departments and professional organizations.
6. Patient-Related Factors
Patient-specific factors such as severe illness, cognitive impairment, low motivation, or lack of interest in learning about their condition can impede education [3] . Hospital stays may be too brief for comprehensive education, or patients may not feel well enough to engage in learning activities.
Recommended approaches: Education should be individualized to the patient’s condition, readiness, and preferences. For those unable to participate fully, involving family or caregivers can ensure information is received and retained. Follow-up after discharge, via phone calls or virtual visits, can reinforce key messages and allow patients to ask questions as they recover.
7. Institutional and Systemic Barriers
Lack of institutional support, insufficient funding for educational programs, and absence of clear policies regarding patient education can reduce the effectiveness of these initiatives [1] . When educational activities are not formally recognized or integrated into workflows, healthcare professionals may deprioritize them in favor of more urgent clinical tasks.
Action steps: Healthcare leaders can advocate for policies that emphasize the importance of patient education, allocate resources for training and materials, and include education as a quality metric in performance reviews. For patients, it may be helpful to ask healthcare providers what educational resources are available and request clarification if information is not provided proactively.
Overcoming Barriers: Practical Steps for Patients and Providers
Overcoming barriers to patient education requires a multifaceted approach. Here are actionable steps for both patients and healthcare professionals:
- Patients : If you experience difficulty understanding health information, let your provider know. Ask for information in simpler terms, request written or visual materials, or involve a trusted friend or family member. If language is a barrier, ask about interpreter services or translated materials. If you feel anxious or overwhelmed, share your feelings with your healthcare team-they can connect you with support resources.
- Healthcare Professionals : Assess each patient’s individual needs, including literacy, language, cultural background, and emotional state. Use multiple teaching methods, verify understanding, and encourage questions. Advocate for institutional resources and policies that support a culture of patient education.
For additional support, consider reaching out to patient advocates, hospital education departments, or community health organizations. Many regions have non-profit groups and public health agencies dedicated to improving patient education. To locate these resources, you can search for “patient education support” or “health literacy programs” in your area, or contact your hospital’s patient services desk.
Key Takeaways
Barriers to patient education are diverse and complex, ranging from practical and systemic to personal and emotional. By recognizing these obstacles and implementing targeted strategies, healthcare providers and patients alike can improve communication, enhance understanding, and achieve better health outcomes. Remember: effective patient education is a partnership-active engagement and open communication are the first steps to overcoming any barrier.

Source: venngage.com
References
- [1] PMC (2025). Barriers and facilitators to patient education from nursing perspectives.
- [2] F. Learning Studio (2024). 6 Barriers to Patient Education and How to Overcome Them.
- [3] Journal of Nursing Practice (2023). Understanding the Barriers Towards Delivery of Patient Education.
- [4] WithPower (2023). 5 Common Barriers to Patient Education and How to Overcome Them.
- [5] PMC (2012). Nurses’ attitude to patient education barriers in educational hospitals.
MORE FROM 9scholarships.de